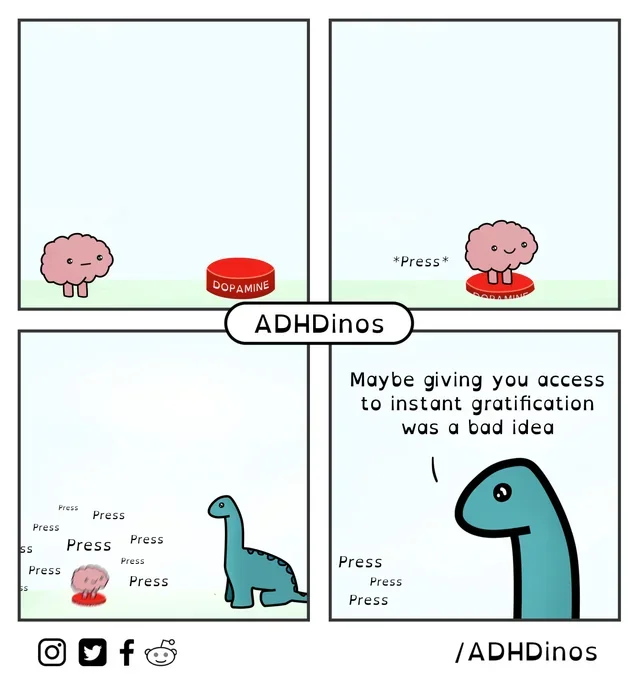
Meandering about the ways that both unconscious and conscious
compulsions can keep us coming back to various substances and
activities that we may or may not want to continue interacting with.
Image courtesy of ADHDinos, check out their comics!
Addiction and Self-Regulation
A practical 2-page guide (inspired by Dopamine Nation + neuroscience)
Mental Meanderings | www.livingcatalyst.org/mentalmeanderings
Quick takeaways
· Addiction is a learning disorder: the brain over-values a reward and under-values everything else.
· Dopamine is more about wanting and reinforcement than simple pleasure - it teaches the brain what to chase next.
· Repeated high-reward exposure shifts your baseline: less joy from normal life, more discomfort when not using.
· Self-regulation improves fastest when you change your environment + add supports (not just 'try harder').
If you may have dangerous withdrawal (alcohol, benzos, some meds), do not stop suddenly - get medical help.
What addiction does to the brain
· The reward circuit (VTA -> nucleus accumbens -> prefrontal cortex) uses dopamine to tag experiences as 'important' and worth repeating.
· Drugs, gambling, porn, ultra-processed foods, endless scrolling, and binge gaming can deliver high-intensity reward signals - fast, frequent, and predictable.
· With repetition, the brain adapts: tolerance (need more for the same effect), withdrawal (feel worse without it), and stronger cue-triggered craving.
The pleasure-pain seesaw (Anna Lembke’s big idea)
· Pleasure and pain are linked in the brain. A big dopamine 'up' is often followed by a compensating 'down' (irritability, anxiety, flat mood). Homeostasis at work.
· If you keep chasing the up, the brain defends itself by tilting toward pain: the baseline drops (anhedonia), and you need the behavior just to feel normal.
· Paradox: short-term relief can create long-term discomfort - which then drives more use.
The addiction cycle (why cravings return)
· Binge / intoxication: the reward becomes the main priority.
· Withdrawal / negative affect: stress systems turn up; relief becomes the goal.
· Preoccupation / anticipation: cues + memories hijack attention and planning.
Why willpower isn't enough
· The prefrontal cortex (planning, inhibition) is easily weakened by stress, sleep loss, pain, hunger, and strong emotion.
· Cues are powerful: people, places, time of day, and even feelings can become automatic triggers.
· Shame fuels secrecy, which fuels relapse. Recovery works better in the open.
----------------------------------------
Self-regulation toolkit: build a plan that wins
· Make the 'good' easy and the 'bad' hard: change cues, add friction, reduce access.
· Start with one target behavior (the biggest pain-to-payoff ratio). Track it - data beats vibes.
· Aim for progress, not perfection. If you slip, treat it as a learning experience, not a failure.
A 30-day reset (Lembke-style)
1. Pick one high-dopamine behavior to pause for 30 days (substance or process addiction).
2. Remove cues: delete apps, change routes, clean the house, avoid high-risk people/places.
3. Expect discomfort days 1-14 (restlessness, low mood, cravings). This is your brain rebalancing.
4. Add 'healthy pain': exercise, cold exposure, hard conversations, service, learning - effort-based rewards.
Tip: Pair abstinence with support (therapy, groups, peer support, trusted friends).
Craving first aid (use one in the moment)
· The 10-minute delay: set a timer, breathe, and promise yourself you can choose again when it ends.
· Urge surfing: notice the urge rise, peak, and fall like a wave (most urges pass if you don't feed them).
· HALT check: Am I Hungry, Angry, Lonely, or Tired? Fix the state before you judge the craving.
· Swap the stimulus: water + protein, a short walk, a shower, a text to someone safe, or change rooms.
Evidence-based help (stronger than white-knuckling)
· Medications can save lives. For opioid use disorder: buprenorphine, methadone, or naltrexone. For alcohol use disorder: naltrexone, acamprosate, or disulfiram (ask a clinician).
· Skills-based therapies (CBT, ACT, motivational interviewing), mutual-help groups (AA/NA, SMART), and recovery coaching/peer support improve outcomes.
· If you use to manage trauma, anxiety, or depression, treating the 'why' reduces relapse risk.
When to get urgent help
· Possible dangerous withdrawal (alcohol, benzodiazepines): tremor, confusion, hallucinations, seizures - seek medical care.
· Overdose risk, suicidal thoughts, or inability to stay safe: call/text 988 (U.S.).
Resources
· SAMHSA National Helpline: 1-800-662-HELP (4357) - free, confidential treatment referrals (24/7).
· FindTreatment.gov - treatment locator (U.S.).
· Talk to your primary care clinic or behavioral health provider about options near you.
Educational handout - not medical advice. If you have symptoms of withdrawal or emergency risk, seek immediate care.
Sources for Handout
Lembke, A. (2021). Dopamine Nation: Finding balance in the age of indulgence. Dutton.
National Institute on Drug Abuse. (2020, July 6). Drugs, brains, and behavior: The science of addiction (online publication). National Institutes of Health.
Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic advances from the brain disease model of addiction. New England Journal of Medicine, 374(4), 363–371. https://doi.org/10.1056/NEJMra1511480
Koob, G. F., & Le Moal, M. (2001). Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology, 24(2), 97–129. https://doi.org/10.1016/S0893-133X(00)00195-0